Policy update 2024: 3 signatures, 1 veto
This legislative cycle, San Francisco AIDS Foundation co-sponsored a total of four bills related to our work. All four were passed by the California state legislature, and all but one received a signature from Governor Gavin Newsom. Here’s what they were, and how they fared, plus info about three other bills of note.
Good news! SB 1333 signed into law
SB 1333, introduced by Senator Susan Eggman and Senator Richard Roth, was signed into law by Governor Newsom on September 22. The “Communicable diseases: HIV reporting” bill will help facilitate the linkage and coordination of HIV care by changing local and state requirements around personally identifying health information–particularly when coinfections are involved.
Why did we need this law?
The need for updated legislation was made clear during the mpox outbreak of 2022–when California’s local and state public health officials were unable to effectively track HIV and mpox co-infections. Only HIV alone (or HIV and certain co-infections) are specified in a statute that allows information to be disclosed for public health tracking purposes–and because mpox was not one of the specified conditions, officials were unable to track and share information about how mpox was affecting people living with HIV. Now, the California Department of Public Health and local health departments will be able to more effectively share public health records in order to link or engage people living with HIV in care.
SB 1333 is sponsored by APLA Health, the California Legislative LGBTQ Caucus, Equality California, and San Francisco AIDS Foundation.
Good news! SB 957 signed into law
Introduced by Senator Scott Wiener, SB 957 requires the California Department of Public Health to collect sexual orientation and gender identity (SOGI) data from third-party entities, including local health jurisdictions (unless prohibited by federal or state law). The bill also speaks to accountability, by requiring CDPH to provide an annual report to the public and California state legislature on its efforts to collect, analyze, and report on SOGI data. Read the press release.
Why did we need this law?
We know that LGBTQ+ populations are disproportionately affected by many health conditions. HIV, for instance, disproportionately affects gay and bisexual men who have sex with men, and transgender individuals. When informed in a timely way about how certain health conditions affect different populations, health care providers can tailor their prevention, testing, outreach, and care. Without an accurate accounting of SOGI data, however, LGBTQ+ communities and the health disparities they face may become invisible or overlooked. Previous legislation has required CDPH to collect SOGI data; this new legislation expands these efforts.
SB 957 is sponsored by Equality CA, California LGBTQ Health & Human Services Network, and San Francisco AIDS Foundation.
Good news! AB 2258 signed into law
AB 2258, introduced by Assemblymember Rick Zbur, will help ensure that preventative services, including PrEP and HIV testing, remain affordable for consumers. The new law will help ensure that health insurance companies cover essential services that are needed in order to deliver recommended preventive services without copays or out-of-pocket costs.
Why did we need this law?
Cost can be a barrier to healthcare. In order to ensure that the most number of people can benefit and access services like PrEP, contraceptives, and HIV and STI screenings, these services should be provided without any out-of-pocket costs. Previous Federal guidance under the Affordable Care Act (ACA) has specified that health insurance companies must cover preventive care without out-of-pocket costs; AB 2258 codifies this federal guidance into California law.
AB 2258 is sponsored by Insurance Commissioner Ricardo Lara, Equality CA, APLA Health, Los Angeles LGBT Center, and San Francisco AIDS Foundation.
Disappointing news: SB 966 vetoed
Governor Newsom vetoed SB 966, introduced by Senator Wiener and sponsored by California Pharmacist Association, California Chronic Care Coalition, the Los Angeles LGBT Center, and San Francisco AIDS Foundation.
This legislation would have regulated pharmacy benefit managers (PBMs), which are intermediaries between insurance companies and drug manufacturers. CVS Caremark, Express Scripts, and Optum Rx are three of the largest PBMs in the industry, according to Cal Matters, and their behind-the-scenes work to negotiate the price of medications, control the list of drugs that insurance plans offer, and process claims is recognized as one source of rising prescription drug costs.
Had it been signed into law, SB 966 would have helped to rein in these rising costs by regulating the ways in which PBMs operate. For instance, it would have prevented “spread pricing,” where PBMs charge more for a drug than it pays a pharmacy, and it would have required that PBMs pass on cost savings negotiated through drug rebates to patients.
”This veto is a massive fail,” said Senator Wiener in a press release issued the day of the veto. “As long as PBMs remain virtually unregulated, and as long as they have an incentive to push expensive name brand drugs, the health plans they control will not cover CalRx’s insulin and most patients won’t access it. Californians will continue to suffer from skyrocketing drug prices, including the 3 million Californians living with diabetes.”
Other bills of note:
VETO: Condom access in public high schools, SB 954. Authored by Senator Caroline Menjivar, this bill would have expanded access to condoms in public high schools in order to curb rising rates of STIs.
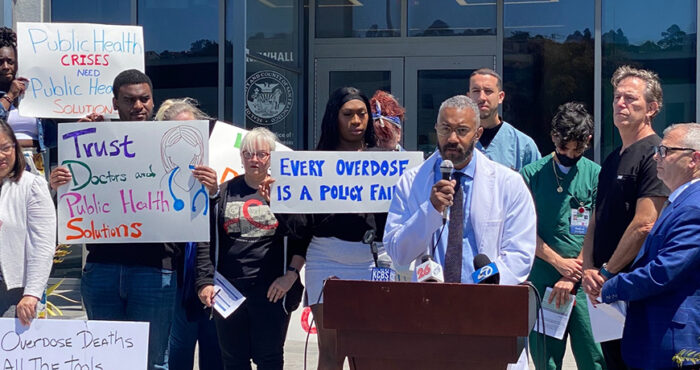
PASS: Expanding drug checking, AB 2136. Authored by Assemblymember Reggie Jones-Sawyer, this bill will help facilitate the expansion of drug checking services, which provide people who use drugs information about the chemical content of their supply (which can help to prevent overdose).
PASS: Expanding methadone access, AB 2115. Authored by Assemblymember Matt Haney, this bill will help to expand methadone treatment, by allowing doctors to prescribe people with up to 72 hours worth of medication to take home, faster entry into treatment programs, and removing barriers to care.