Two studies share insights into Doxy PEP use in San Francisco
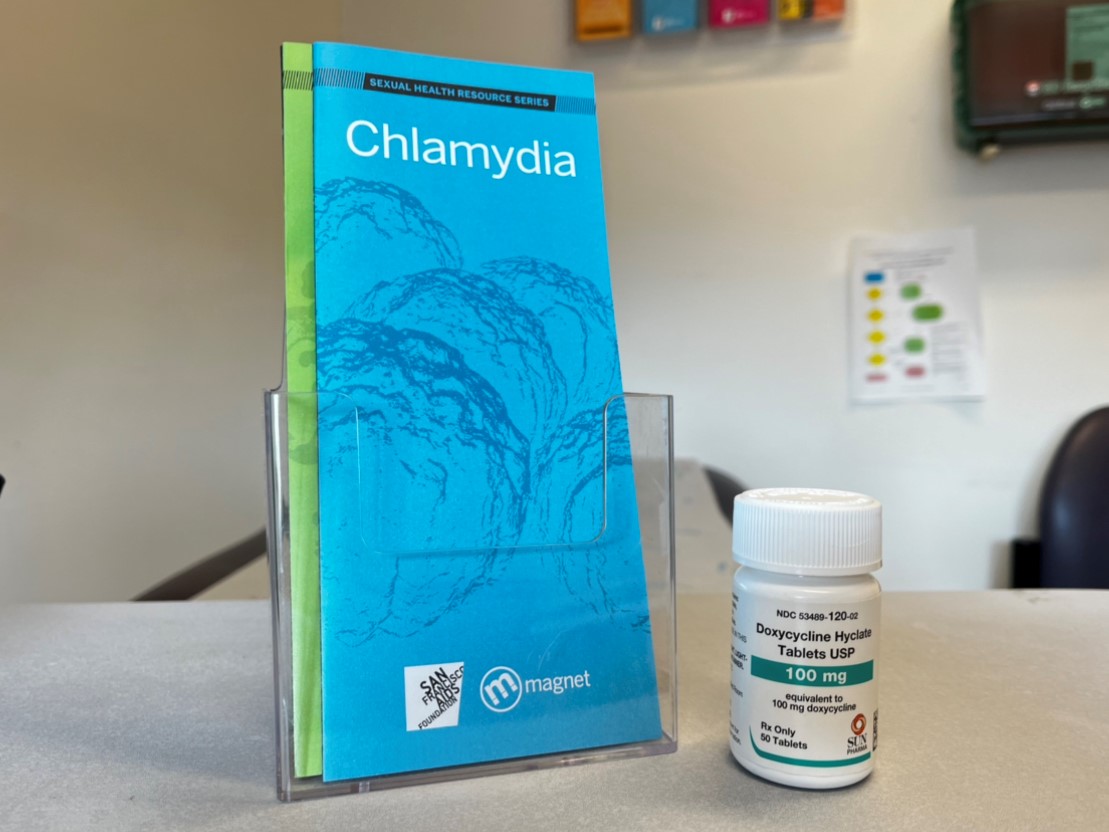
Two studies presented at the Conference on Retroviruses and Opportunistic Infections (CROI) 2025 shared the impact and uptake of the STI prevention method Doxy PEP among clients at SFAF’s sexual health clinic Magnet. Although overall uptake and consistent adherence among eligible clients is relatively low, STI incidence is falling with significant declines in gonorrhea, chlamydia, and syphilis cases among people who do report using this prevention strategy.
Hyman Scott, MD, MPH, SFAF’s medical director and the clinical research medical director of SFDPH’s Bridge HIV clinic compared STI incidence during the time period prior to the Doxy PEP program beginning to the time period following Doxy PEP’s availability at the clinic, between PrEP clients who used Doxy PEP and those who did not use Doxy PEP. More than 4,500 were included in the analysis (2,525 Doxy PEP users; 2,068 non-users).
People who ended up taking Doxy PEP were nearly four times likely to be diagnosed with an STI during the pre-Doxy PEP time period compared to those who never ended up taking Doxy PEP, indicating that people who were most at risk for STIs were the individuals who ended up taking Doxy PEP.
There were significant declines in STI incidence after Doxy PEP roll-out among clients taking Doxy PEP, but not among non-Doxy PEP users. Prior to Doxy PEP becoming available, there was a steep increase in STIs experienced by people who would become Doxy PEP users, and a slight decline in STIs among people who never ended up using Doxy PEP.
For people taking Doxy PEP, there was a significantly reduced likelihood of a diagnosis with any STI (66% reduction) or with chlamydia (81% reduction), syphilis (89% reduction), or gonorrhea (44% reduction) during the post-Doxy PEP implementation time period than compared to the time before Doxy PEP became available.
“This is similar to the efficacy that has been seen in clinical trials,” said Scott. “And this is one of the first analyses that has shown a nearly 50% decline in gonorrhea incidence in a setting of clinical implantation of Doxy PEP.”

Mike Barry, SFAF’s director of evaluation & impact, shared data on the uptake and use of Doxy PEP among 7,436 Magnet clients between December 2022 (when the Doxy PEP program began) to December 2024.
Of the 7,436 clients who had an indication for Doxy PEP, more than half (59%, or 4,369 people) received a prescription; 61% (2,651) of those individuals reported taking one or more doses, and 61% (1,627) of individuals who took one or more doses reported high adherence (22% of all clients indicated for Doxy PEP).
Barry explained that although the number of people in the “high adherence” group seems low, it’s possible that clients are savvy users of Doxy PEP–and opt to take the medication during sexual encounters that are highest risk and forgo use of the medication in lower-risk situations. By, for instance, using Doxy PEP after a sex party but forgoing the medication after sex with regular partners.
There were notable differences in prescription receipt by group, with fewer prescriptions among younger individuals, transgender men, unhoused and unstably housed individuals, and HIV-negative individuals not using PrEP. Transgender women were more likely to be prescribed Doxy PEP than individuals of other gender identities. Younger individuals, Black and African American individuals, unhoused or unstably housed individuals, and people living with HIV were less likely to initiate Doxy PEP once prescribed. Young individuals and people living with HIV were less likely to report high adherence if they took Doxy PEP at least once.
Younger individuals ages 14-29, Black and African American clients, people who reported unstable housing or homelessness, and clients living with HIV were less likely to report high adherence.
“We approached this research with the goal of informing our provision of sexual health care,” said Barry. “Knowing the social determinants of health that affect Doxy PEP uptake and adherence will directly inform our ability to intervene and tailor prevention services, so that all communities are able to benefit equitably from this prevention measure.
References
Scott, H., Roman, J, Spinelli, A., Bena, J., Barry, M., Heise, M., Buchbinder, S. (2025). High sustained effectiveness of Doxycycline PEP for STI prevention after clinical implementation. CROI 2025, Abstract 163.
Barry, M., Bena, J. Roman, J., Scott, H. (2025). The Doxy-PEP continuum among patients receiving care at a sexual health clinic in San Francisco. CROI 2025, Abstract 164.










