“Substantial and sustained” decline in chlamydia and syphilis among Doxy PEP users in Northern California

Two new studies published in JAMA Internal Medicine give more evidence about the effectiveness of Doxy PEP to prevent sexually transmitted infections in “real-world” patient populations–this time with people using Doxy PEP who are part of Kaiser Northern California’s PrEP program, and city-wide across San Francisco among men who have sex with men and trans women.
Both studies found significant reductions in chlamydia and syphilis over their respective study periods, with less of an effect or no effect on gonorrhea infections.
“We’ve known from clinical trials that Doxy PEP can work for individuals to prevent bacterial STIs,” said Jorge Roman, MSN, FNP-BC, AAHIVS, senior director of clinical services at SFAF. “But what we really want to know is – can Doxy PEP work to bring down STI infections across an entire population? Finding that out was the goal of these studies.”
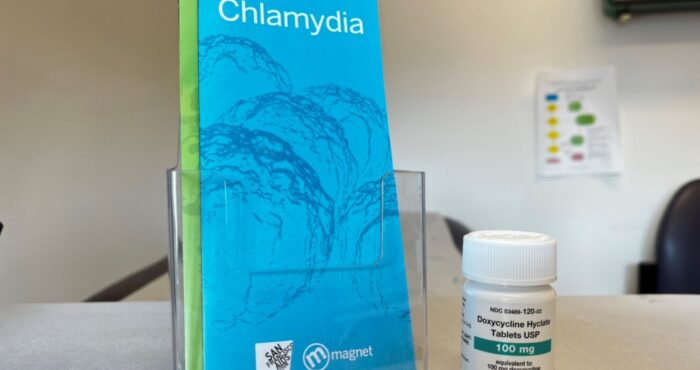
Doxy PEP is an STI prevention strategy that involves taking 200 mg of the antibiotic doxycycline “Doxy” within 24 to 72 hours of sex to prevent STIs. Soon after the San Francisco Department of Public Health began recommending Doxy PEP for certain populations including cis men and trans women with a history of bacterial STIs and condomless sex, in October 2022, local clinics began prescribing Doxy PEP to clients.
A study by Madeline Sankara, MPH, and colleagues speaks to the impact of Doxy PEP on an entire population of people seeking STI care in San Francisco. By analyzing data collected on STI diagnoses (mandated for public health surveillance) researchers were able to see “substantial and sustained” declines in chlamydia and syphilis (but not gonorrhea) among men who have sex with men and trans women city-wide after the implementation and scale-up of Doxy PEP programs.
From November 2022 to December 2023, a total of 3,974 men who have sex with men and trans women started Doxy PEP at three San Francisco sexual health clinics (SFAF’s clinic, Magnet; City Clinic; and Ward 86).
The researchers compared STI cases from July 2021 – October 2022 (pre-Doxy PEP) to November 2022 – November 2023 (post-Doxy PEP), looking specifically at gonorrhea, syphilis, and chlamydia cases among men who have sex with men and transgender women.
Stephanie Cohen, MD, the lead researcher on the study, explained that they used mathematical modeling to predict what STI case counts would have looked like if the trends in STIs had stayed the same, and compared those to what actually happened in the months following the release of the Doxy PEP guidelines.
They found that by November 2023 (13 months after the Doxy PEP guidelines were released in San Francisco), there was an approximately 49% reduction in chlamydia cases, a 51% reduction in early syphilis cases, and a 25% increase in gonorrhea cases compared with the number of cases pre-Doxy PEP.
At the same time, chlamydia cases among cisgender women increased significantly (cis women are not recommended to take Doxy PEP).
The researchers note the “substantial and sustained” declines in chlamydia and early syphilis cases among men who have sex with men and trans women in San Francisco after Doxy PEP was introduced, leading them to conclude that the declines were “at least in part” due to Doxy PEP use.
There was no decrease in gonorrhea infections among men who have sex with men and trans women after Doxy PEP’s introduction into the community.
Cohen explained that this is an ongoing area of investigation, but that the “most likely” explanation is that the gonorrhea strains in San Francisco–and circulating nationally–may be resistant to the tetracycline class of antibiotics that doxycycline is in.
“That’s something that was already known about gonorrhea before all of this work on Doxy PEP began,” she said.
A different study by Michael Traeger, PhD, MSc, and colleagues, analyzed data on STI diagnoses among Kaiser Northern California PrEP users who were offered Doxy PEP starting in November 2022.
The number of diagnoses of chlamydia, gonorrhea, and syphilis were compared among people who opted to take Doxy PEP before and after Doxy PEP became available, and between the group of people who opted to take Doxy PEP and the group of PrEP users who did not take Doxy PEP.
Among the group of 2,253 people who were dispensed Doxy PEP at least once, the average chlamydia “positivity” (measured every three months) declined from 9.6% in the two years before Doxy PEP to 2.0% in the year following. Significant declines occurred in rectal, urethral, and pharyngeal (throat) infections (all three anatomical sites that are tested).
Syphilis infections showed a similar dramatic downward trend, with average positivity declining from 1.7% before Doxy PEP to 0.3% in the year afterward.
There was a decline in average gonorrhea positivity before and after Doxy PEP, from 10.2% to 9.0%, with statistically significant declines in rectal and urethral infections but not pharyngeal (throat) infections.
The group of individuals who opted to take Doxy PEP had higher rates of gonorrhea, chlamydia, and syphilis before taking Doxy PEP than the group of individuals who did not take Doxy PEP, which helps to confirm intuitively that individuals who were more at risk for STIs were the ones who opted to take Doxy PEP. (Nearly half–48.6%–of people who took Doxy PEP had any STI in the previous 12 mos before beginning Doxy PEP, compared to 18.2% of people who did not take Doxy PEP.)
This risk dropped, however, with the use of Doxy PEP–at least for chlamydia and syphilis. Doxy PEP recipients had lower chlamydia and syphilis positivity after beginning this STI prevention medication than the people who never took Doxy PEP. The group of people who did not take Doxy PEP had stable rates of chlamydia, syphilis, and gonorrhea during this time period.
Interestingly, there were greater declines in STI positivity rates among clients specifically in San Francisco compared to the greater Bay Area. Because other non-Kaiser San Francisco Doxy PEP programs scaled up during the study period (e.g., SFAF’s Magnet clinic, City Clinic), the authors hypothesize that there may have been a compounding benefit to “wider doxyPEP implementation for interrupting STI transmission in sexual networks of people using HIV PrEP.”
This study, as in previous studies, found Doxy PEP to be associated with significant protection against syphilis and chlamydia, but only moderately protective against gonorrhea infections (but not pharyngeal/throat gonorrhea). The researchers explain that some level of gonorrheal antibiotic resistance present in the population may be to blame, and note that ongoing monitoring for resistance in gonorrhea will be important.
These studies provide welcome information about the effectiveness of Doxy PEP to reduce chlamydia and syphilis infections, but leave the door open for future studies.
“I can’t overstate the importance of having a prevention tool for all populations in all gender categories, including cisgender women as well as more research that’s inclusive of transgender and non-binary populations,” said Cohen.